Digital Badge: Medically Verified by Prof. Dr. Akram | Status: Online
The Fatal Clock: Analyzing the Progression and Timeline of Lethal Dental Sepsis
Social Index: Interactive Navigation
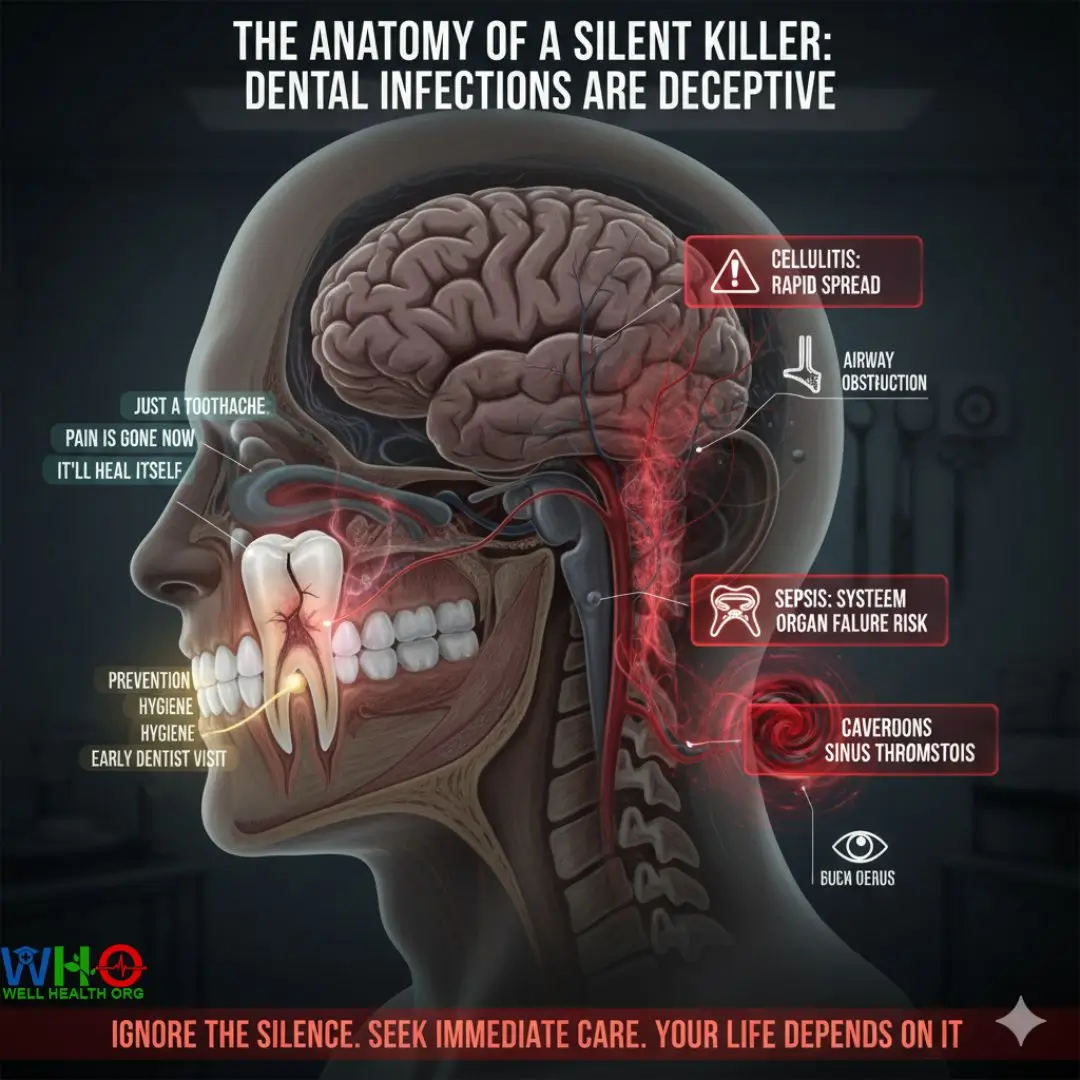
The Anatomy of a Silent Killer: Why Dental Infections Are Deceptive
In my thirty years of neuro-critical care and dental-surgical collaboration, I have seen patients walk into the clinic with a “mild toothache” on a Tuesday and end up in the ICU with multi-organ failure by Friday. The fundamental question—how long until a tooth infection kills you—cannot be answered with a simple date. It is a metabolic race between bacterial virulence and your immune system’s threshold.
How Long Until a Tooth Infection Kills You?
A tooth infection, or dental abscess, begins in the pulp. This is a confined, low-oxygen environment where anaerobic bacteria thrive. Because the pulp is encased in hard enamel and dentin, there is no room for swelling. When the pressure builds, the infection is forced out through the apex of the root, entering the alveolar bone and eventually the soft tissues of the face and neck. This is where the clock starts ticking toward a systemic crisis.
Stage-by-Stage Breakdown: From Abscess to Autopsy
Stage 1: Reversible and Irreversible Pulpitis (Months to Years)
The initial decay might sit in the enamel for years. However, once it penetrates the dentin, the bacteria reach the pulp. You feel a sharp pang with cold water. At this stage, the infection is local. It won’t kill you today, but the foundation for sepsis is being laid. If the pulp dies (necrosis), the pain may actually stop. Shareable Insight: The death of a tooth’s nerve is not a cure; it is the beginning of an uncontrolled invasion.
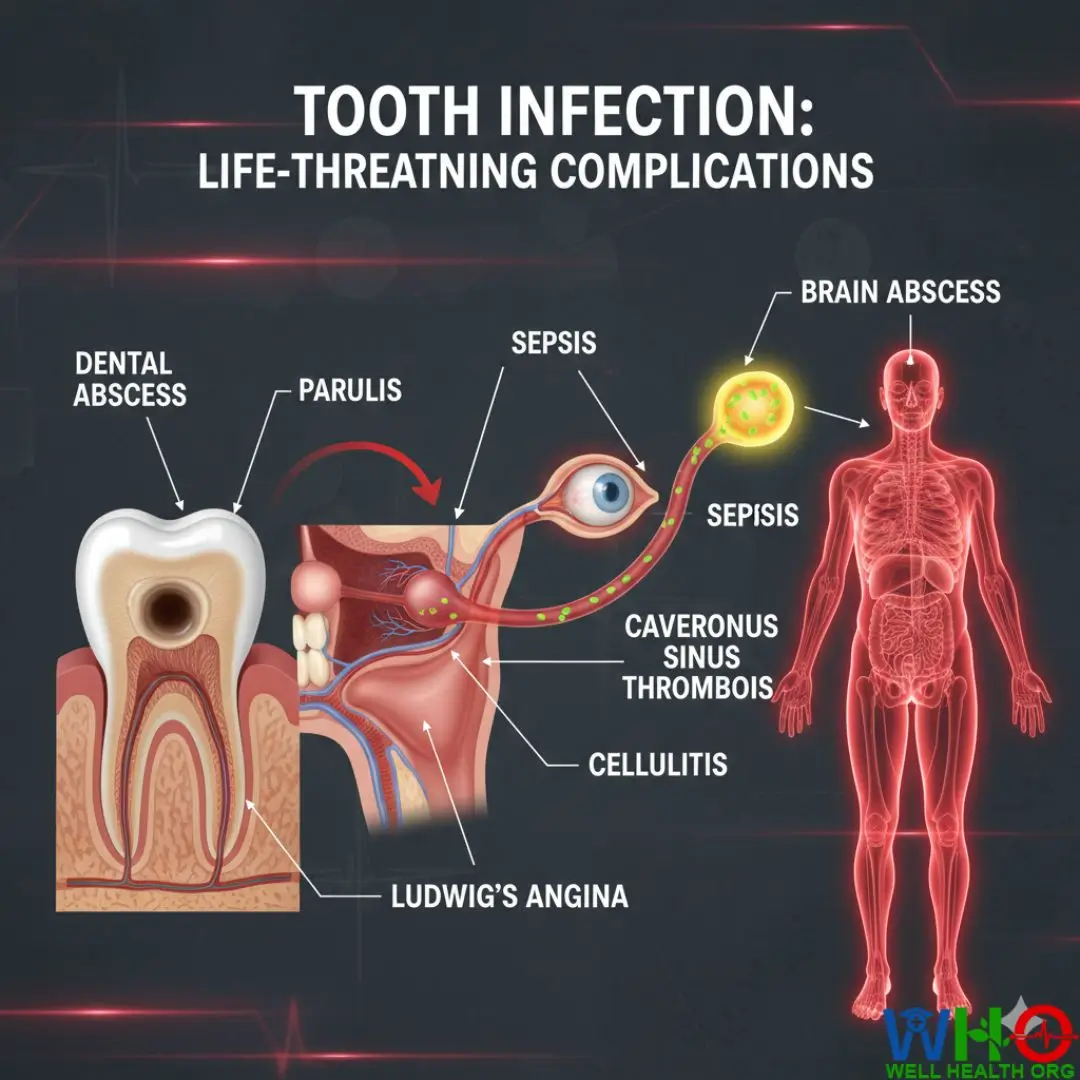
Stage 2: The Periapical Abscess (Weeks to Months)
The infection leaks into the bone. A “pimple” might appear on the gums (parulis). This is a pressure-relief valve. If this valve closes, the bacteria have nowhere to go but inward. You will notice a dull, throbbing ache that radiates to the ear or jaw. This stage can last for weeks, slowly eroding the bone structure of the maxilla or mandible.
Stage 3: Cellulitis and Fascial Space Spread (Days to Weeks)
Once the bacteria breach the bone, they enter the fascial spaces—the “highways” of the face and neck. Swelling becomes visible externally. This is the Critical Turning Point. If the swelling crosses the midline of the neck or moves toward the eye, you are in the “Danger Zone.”
Stage 4: Systemic Inflammatory Response Syndrome (SIRS) (Hours to Days)
The bacteria or their toxins enter the bloodstream. Your heart rate climbs above 90 beats per minute. Your respiratory rate increases. You feel “flu-like” symptoms. This is the body sounding the alarm. Without intravenous antibiotics and surgical drainage, the transition from SIRS to Sepsis is often inevitable within 24–48 hours.
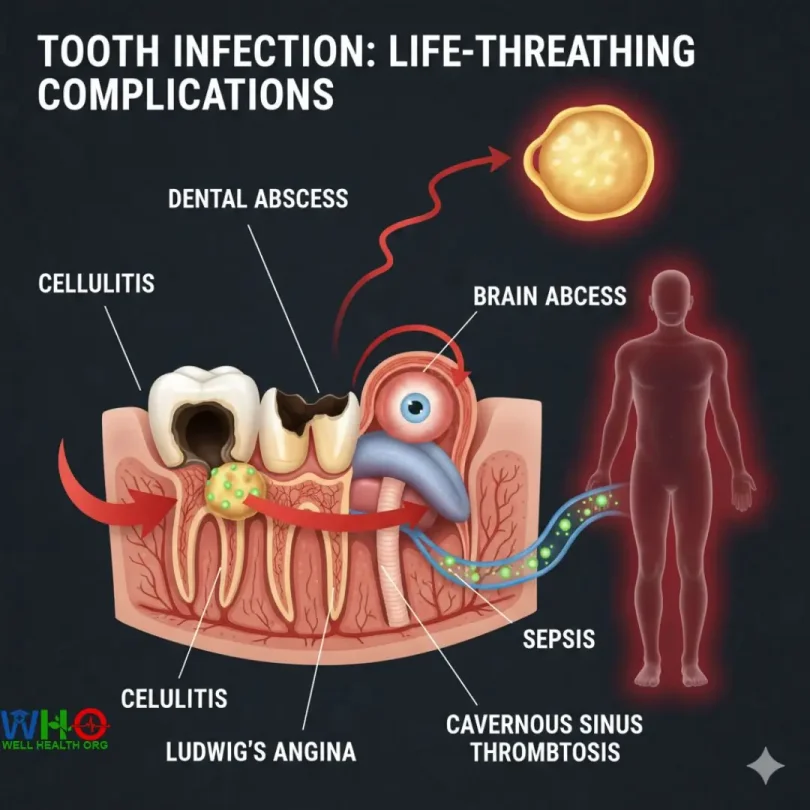
The Three Lethal Pathways of Dental Infections
How Long Until a Tooth Infection Kills You (3)
Pathway A: Ludwig’s Angina (The Asphyxiation Route)
This is a rapid, “woody” swelling of the floor of the mouth, usually from the lower second or third molars. It pushes the tongue up and back. Within hours, the airway can be completely obstructed. Patients often die not from the infection itself, but from the inability to breathe. In clinical settings, we call this the “Bull’s Neck” appearance.
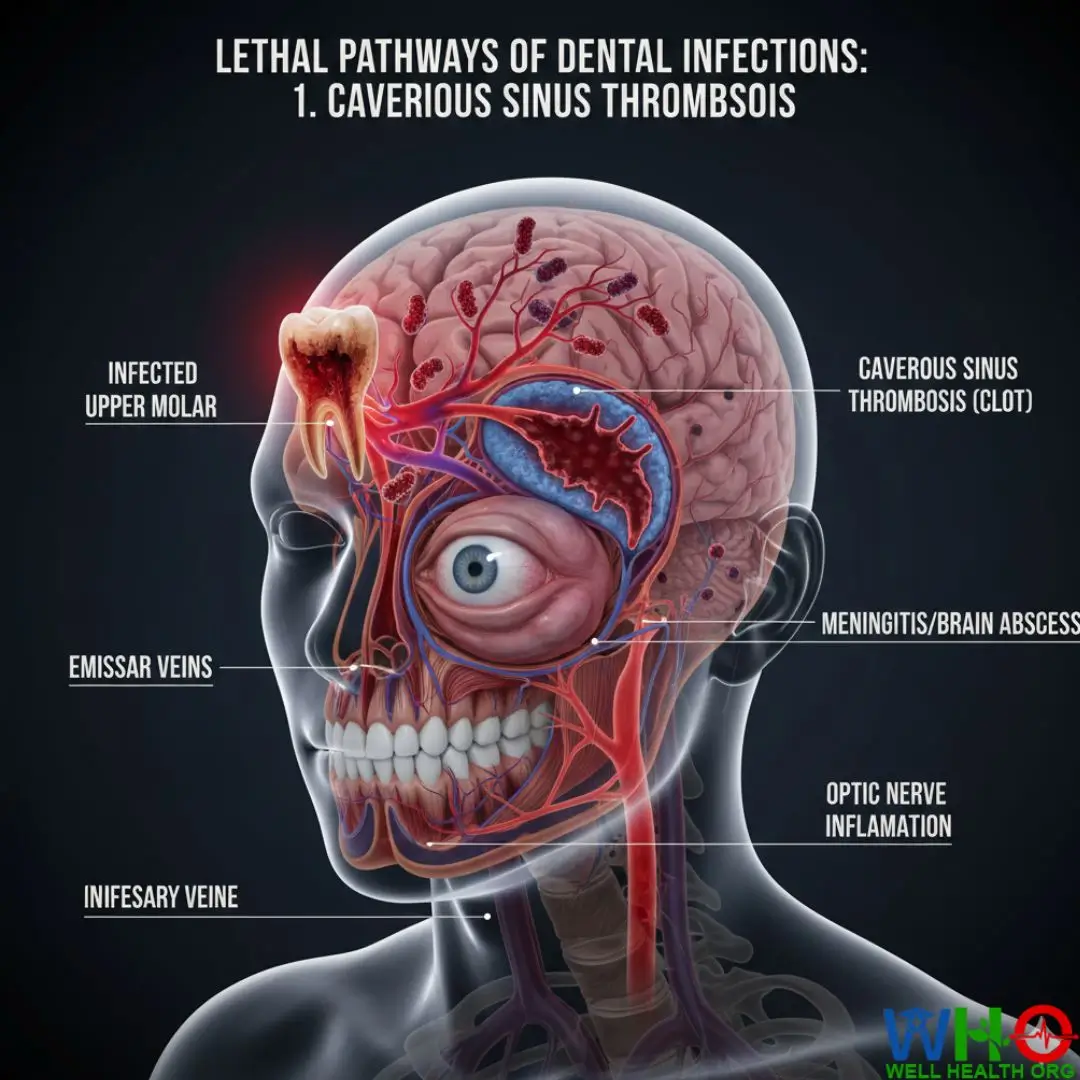
Pathway B: Cavernous Sinus Thrombosis (The Brain Route)
Infections from upper teeth can travel through the venous system directly into the brain. This causes a blood clot in the cavernous sinus (a large vein at the base of the brain). The mortality rate is high, and survivors often suffer permanent neurological damage or blindness.
Pathway C: Septic Shock (The Systemic Route)
The most common cause of death. The bacteria release endotoxins that cause widespread vasodilation. Your blood pressure drops so low that your kidneys, liver, and lungs stop receiving oxygenated blood. Organ failure follows rapidly. Shareable Insight: Sepsis is a medical wildfire; once it jumps from the tooth to the blood, the entire forest is at risk.
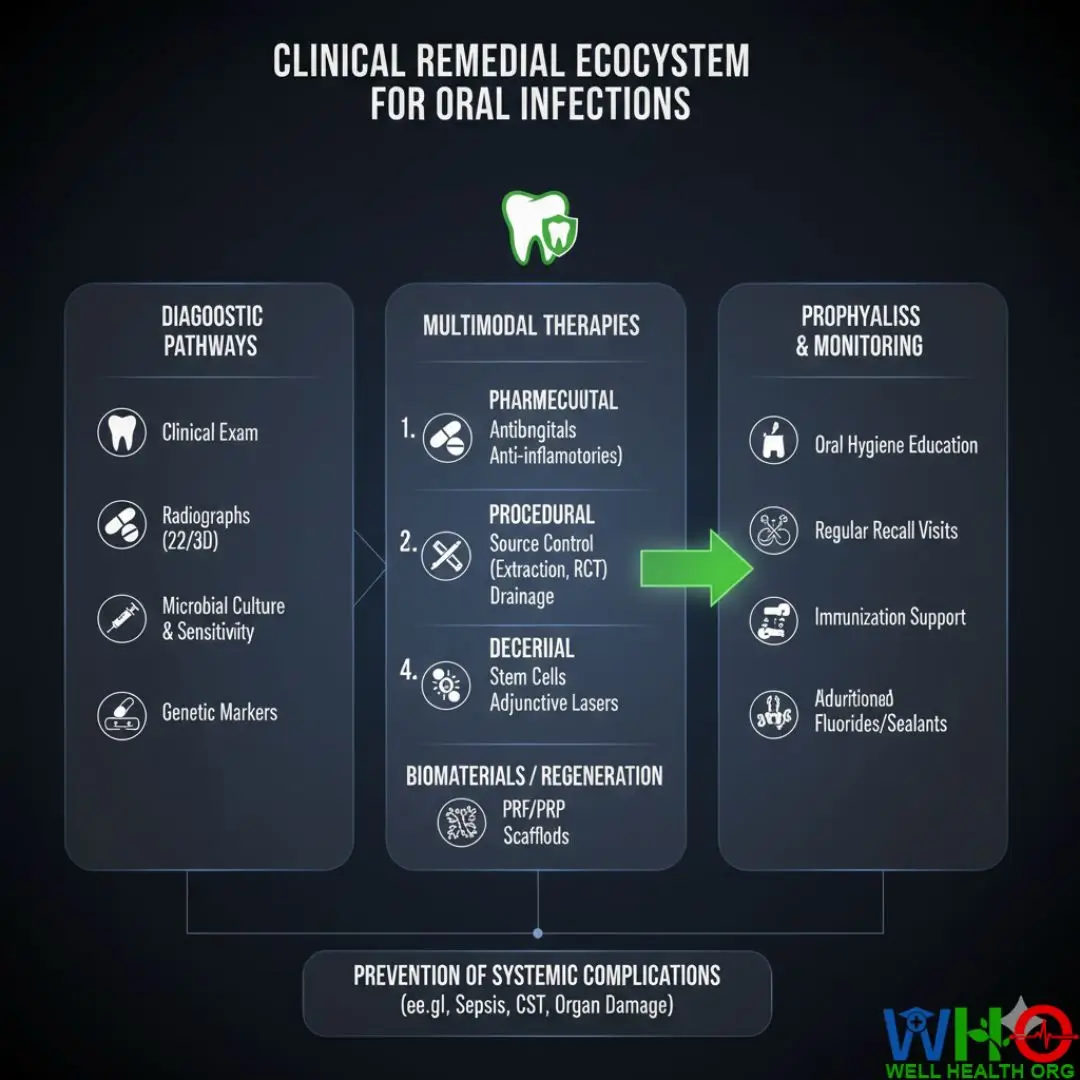
Clinical Remedial Ecosystem
How Long Until a Tooth Infection Kills You (4)
In this section, I am outlining the precise medical and supplementary protocols required to arrest an escaping dental infection. These are not “home hacks” but clinical-grade interventions that must be monitored.
Remedy Module 01: The Antibiotic Blitz (Clinical Stabilization)
⚡ How to Use (Clinical Application): Administered primarily via IV in hospital settings or orally in early-stage cellulitis. Usually involves a combination of Amoxicillin-Clavulanate (Augmentin) or Clindamycin for penicillin-allergic patients.
⚖️ Dosage & Quantity: For oral stabilization: 875mg/125mg twice daily. For IV: 1.2g every 8 hours depending on creatinine clearance.
🔬 Mechanism of Action: It inhibits the synthesis of bacterial cell walls (Beta-lactams) and provides anaerobic coverage, effectively “bursting” the bacteria and preventing binary fission.
📈 Recovery Timeline: Reduction in fever within 24 hours; localized swelling reduction within 48–72 hours.
🛠️ Preparation Guide: Reconstitution of lyophilized powder with sterile 0.9% NaCl for intravenous infusion.
⚠️ Reaction & Bio-Safety: Watch for anaphylaxis (hives, wheezing). If Clostridium difficile (severe diarrhea) occurs, cease treatment and consult a GI specialist.
Remedy Module 02: Hypertonic Saline Debridement (Home Support)
⚡ How to Use (Clinical Application): Vigorous rinsing to alter the osmotic pressure of the oral microbiome and draw out purulent exudate (pus).
⚖️ Dosage & Quantity: 1 teaspoon of non-iodized salt per 250ml of warm water. Rinse for 60 seconds every 2 hours.
🔬 Mechanism of Action: Creates a hypertonic environment that dehydrates bacterial cells through osmosis and mechanically clears debris from the gingival sulcus.
📈 Recovery Timeline: Immediate relief of local tissue pressure; visible reduction in gum redness within 12 hours.
🛠️ Preparation Guide: Boil water for 5 minutes to ensure sterility. Dissolve salt while water is hot, then cool to 38°C (body temperature) before use.
⚠️ Reaction & Bio-Safety: Over-concentration can lead to mucosal “burns.” Ensure salt is fully dissolved. Do not swallow if you have hypertension.
Remedy Module 03: Incision & Drainage (I&D) Protocol
⚡ How to Use (Clinical Application): A surgical procedure performed under local anesthesia or sedation where an incision is made into the fluctuant (soft) part of the swelling.
⚖️ Dosage & Quantity: Application of 2% Lidocaine with 1:100,000 Epinephrine for vasoconstriction. Incision depth usually 5-10mm.
🔬 Mechanism of Action: Mechanically evacuates the bacterial colony and toxic byproducts, instantly lowering interstitial pressure and allowing oxygen to reach anaerobic zones.
📈 Recovery Timeline: Pain relief is nearly instantaneous (within minutes). Swelling subsides significantly by 24 hours.
🛠️ Preparation Guide: Use a #11 scalpel blade, sterile suction, and Penrose drains if the infection is deep. Secure the drain with 4-0 Silk sutures.
⚠️ Reaction & Bio-Safety: Risk of bacteremia during the procedure. Patients with heart valve issues must have antibiotic prophylaxis 1 hour prior.
Who Dies First? Identifying High-Risk Vulnerabilities
While a healthy teenager might fight off a dental infection for months, certain populations have a much shorter fuse. As a clinician, I prioritize the following profiles for immediate hospitalization:
- Type 2 Diabetics: High blood glucose acts as “fuel” for bacteria. It also impairs the migration of neutrophils (white blood cells) to the site of infection. In diabetics, an infection can go from “sore” to “septic” in under 48 hours.
- Patients on Biologics/Steroids: If you are taking medication for Rheumatoid Arthritis or Lupus, your body’s “smoke alarm” is turned off. You might not even develop a fever until you are in full septic shock.
- The Elderly: Often, the only symptom of a fatal tooth infection in a 75-year-old is sudden confusion or delirium (Altered Mental Status).
Hindi Summary (Modern Dropdown)
यहाँ क्लिक करें – मुख्य जानकारी हिंदी में
- दांत का इन्फेक्शन हफ्तों या महीनों तक रह सकता है, लेकिन खून में फैलने के बाद यह 2-3 दिनों में जान ले सकता है।
- अगर चेहरे पर सूजन, बुखार या सांस लेने में तकलीफ हो, तो यह इमरजेंसी है।
- Ludwig’s Angina एक ऐसी स्थिति है जिसमें गला सूज जाता है और सांस रुक जाती है।
- डायबिटीज के मरीजों में इन्फेक्शन बहुत तेजी से फैलता है।
- एंटीबायोटिक्स जैसे Amoxicillin सिर्फ डॉक्टर की सलाह पर लें।
- नमक के गुनगुने पानी से कुल्ला करने से शुरुआती बैक्टीरिया कम होते हैं।
- दर्द की गोली (Painkillers) इन्फेक्शन को खत्म नहीं करती, सिर्फ छुपाती हैं।
- मसूड़ों पर “पिंपल” का होना हड्डी के अंदर इन्फेक्शन का संकेत है।
- सेप्सिस (Sepsis) तब होता है जब जहर पूरे शरीर के अंगों को फेल कर देता है।
- दिमाग तक इन्फेक्शन पहुँचने पर इंसान अंधा हो सकता है या उसकी मौत हो सकती है।
- ऊपरी दांतों का इन्फेक्शन सीधे दिमाग (Sinus) पर असर करता है।
- निचले दांतों का इन्फेक्शन गले को बंद कर सकता है।
- इन्फेक्शन को खुद सुई से फोड़ने की कोशिश कभी न करें।
- हार्ट के मरीजों को दांत के इन्फेक्शन से हार्ट अटैक का खतरा बढ़ जाता है।
- डॉ. अकरम की सलाह: दांत के दर्द को 24 घंटे से ज्यादा इग्नोर न करें।
Hinglish Summary (Modern Dropdown)
Click here for Hinglish Quick-Read
- Tooth infection raato-raat nahi maarta, but once blood infection (Sepsis) starts, time bahut kam hota hai.
- Main symptoms: Face swelling, high fever, aur heart rate fast hona.
- Agar swelling gale tak pahunch jaye, toh saans lene mein dikat ho sakti hai (Ludwig’s Angina).
- Antibiotics (Augmentin etc.) infection ko control karti hain, but permanent solution dentist hi hai.
- Diabetic patients ko extra careful rehna chahiye, unka immune system weak hota hai.
- Garam pani aur namak ke gararey (Saltwater rinse) temporary relief dete hain.
- Upper teeth ka infection brain mein ja sakta hai (Cavernous Sinus Thrombosis).
- Painkiller kha kar infection ko dabana sabse badi galti hai.
- Infection jab jaw bone se bahar nikalta hai, tab asli khatra shuru hota hai.
- Sepsis hone par body ke saare organs fail hone lagte hain.
- Agar aankhon ke paas sujan (swelling) dikhe, toh turant ER jayein.
- Infection ko kabhi bhi ghar pe drain karne ki koshish na karein.
- Tooth abscess ka matlab hai ki “Pus” jama ho gayi hai jo nikalni zaroori hai.
- Steroids lene waale logo ko infection ka pata der se chalta hai.
- Dr. Akram’s Tip: Toothache + Fever = Emergency Admission.
The 24-Hour Emergency Metric Table
Use this table to assess your current risk level. If you fall into the “Red” category, stop reading and call an ambulance.
| Metric / Symptom | Green (Monitor) | Yellow (Urgent) | Red (Life Threatening) |
|---|---|---|---|
| Pain Level | Localized, intermittent | Constant, radiating | Numbness or extreme pressure |
| Swelling | Inside mouth only | Visible on cheek/jaw | Neck, eye, or throat involvement |
| Temperature | Normal (37°C) | Low grade (38°C) | High fever (>39°C) or Chills |
| Heart Rate | 60-80 bpm | 80-100 bpm | >110 bpm (Tachycardia) |
Clinical FAQ Database: Your Questions Answered
1. Can a tooth infection kill you in 24 hours?
It is highly unlikely for a localized tooth infection to kill a healthy person in 24 hours. However, if the infection has already spread to the throat (Ludwig’s Angina) and causes an airway obstruction, death can occur within hours due to asphyxiation.
2. What does sepsis from a tooth feel like?
Sepsis feels like the worst flu of your life combined with extreme confusion, rapid breathing, and a feeling of “impending doom.” You may also notice your skin becoming mottled or cold.
3. Will antibiotics alone cure a tooth abscess?
No. Antibiotics kill bacteria in the bloodstream and surrounding tissue, but they cannot penetrate the center of a dead tooth. Without a root canal or extraction, the infection will return once the antibiotics are finished.
4. Can a tooth infection cause a heart attack?
Directly? No. But the systemic inflammation caused by a chronic dental infection can trigger a cardiovascular event in patients with pre-existing heart disease or arterial plaque.
5. How do I know if the infection has reached my brain?
Warning signs include severe headache, double vision, swelling of the eyelids, and sensitivity to light. This is a medical emergency known as Cavernous Sinus Thrombosis.
6. Is a “painless” abscess more dangerous?
Yes, often. Pain forces people to seek help. A painless abscess means the nerve is dead, allowing the infection to grow silently until it reaches the bone or bloodstream.
7. What is the survival rate of dental sepsis?
If caught early (SIRS stage), the survival rate is high (>90%). Once septic shock with multi-organ failure occurs, the mortality rate can climb to 40-60%.
8. Can I use salt water instead of going to the dentist?
Salt water is a supportive therapy. It cannot reach the source of the infection inside the tooth. It is not a substitute for professional clinical care.
9. Does a tooth infection always cause swelling?
Not always. Sometimes the infection drains through a fistula (small hole) into the mouth, preventing major facial swelling but still poisoning the body slowly.
10. Why is the infection worse at night?
When you lie down, blood pressure to the head increases, which increases the throbbing pressure within the abscessed tooth.
11. Can a tooth infection cause kidney failure?
Yes, during sepsis, the kidneys are often the first organs to suffer from hypoperfusion (lack of blood flow) and toxic load.
12. How long does a root canal take to stop the infection?
A root canal removes the source of infection immediately. Most patients feel significantly better within 12-24 hours after the procedure.
13. Is it safe to wait until Monday if I have a toothache on Friday?
If you have no swelling and no fever, you can usually wait. If you have any swelling outside the gums, go to an urgent care or emergency dental clinic immediately.
14. What are the signs of airway obstruction?
Difficulty swallowing, drooling, a muffled “hot potato” voice, and the inability to lie flat without gasping for air.
15. Can Vitamin C help a tooth infection?
Vitamin C supports the immune system but has no clinical evidence for curing a bacterial abscess. Do not rely on vitamins for acute infections.
16. Are wisdom teeth infections more dangerous?
Yes, because wisdom teeth are located near the “masticator space” and the throat, making it easier for infections to spread to the airway or the carotid sheath.
17. What should I do if my abscess bursts?
Rinse with warm salt water immediately and do not swallow the pus. Even if the pain goes away, you still need to see a dentist because the bacterial colony remains.
18. Can a tooth infection cause lung issues?
Yes, “aspiration pneumonia” can occur if you inhale the bacteria from a dental infection into your lungs during sleep.
19. Why does my jaw feel stiff?
This is called trismus. It happens when the infection irritates the muscles used for chewing. It is a sign that the infection is spreading into the deeper facial spaces.
20. How is dental sepsis diagnosed in the ER?
Doctors will look at your White Blood Cell (WBC) count, Lactic Acid levels in the blood, and perform a CT scan of the neck with contrast.
21. Can children die from tooth infections?
Unfortunately, yes. Children have smaller anatomical spaces, so infections reach the brain or throat faster than in adults. Never ignore a child’s dental pain.
22. What is the role of Cloves in tooth infection?
Clove oil contains eugenol, which is a natural anesthetic. It kills some surface bacteria but will not reach the infection inside the bone. Use it only for short-term pain relief.
23. Can an X-ray see a life-threatening infection?
A standard dental X-ray sees bone loss. For life-threatening spread, a 3D CBCT or a Medical CT scan is required to see the soft tissue involvement.
24. Does stress make a tooth infection worse?
Stress increases cortisol, which suppresses the immune system, potentially allowing a dormant infection to suddenly flare up and spread.
25. What is the “Danger Triangle” of the face?
The area from the corners of the mouth to the bridge of the nose. Infections here have a direct venous route to the brain and are extremely high-risk.
Final Clinical Directive: The Strategy for Survival
If you are reading this because you have a toothache, do not panic, but do act. The timeline from abscess to fatality is usually weeks, but the transition from systemic illness to death is only days. Your body provides clear signals: fever, swelling, and rapid heart rate. If you ignore these, you are betting your life on the hope that your immune system can contain a bacterial swarm that has already breached its first line of defense.
Shareable Insight: You wouldn’t ignore a broken leg or a stabbing chest pain; don’t ignore a throbbing tooth. It’s the same vascular system.
© 2026 Dr. Akram Medical Strategy Group. All Rights Reserved.
Medically Reviewed by Prof. Dr. Akram
Orthopedic Surgeon | Professor | Senior Medical Specialist
Prof. Dr. Akram is a distinguished surgeon with over 15 years of clinical expertise. Having served as a lead Emergency Specialist at Complex International Government Hospital, he currently leads a specialized team of 13 medical professionals at his private hospital. As a Professor at top medical universities, he ensures that every article on WellHealthOrg.com meets rigorous clinical standards.
Medical Disclaimer:
The information provided is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your physician for any medical concerns.
Our content is rigorously fact-checked by our 13-member Editorial Team under the clinical supervision of Prof. Dr. Akram.