Introduction Syphilis False-Positive Tests
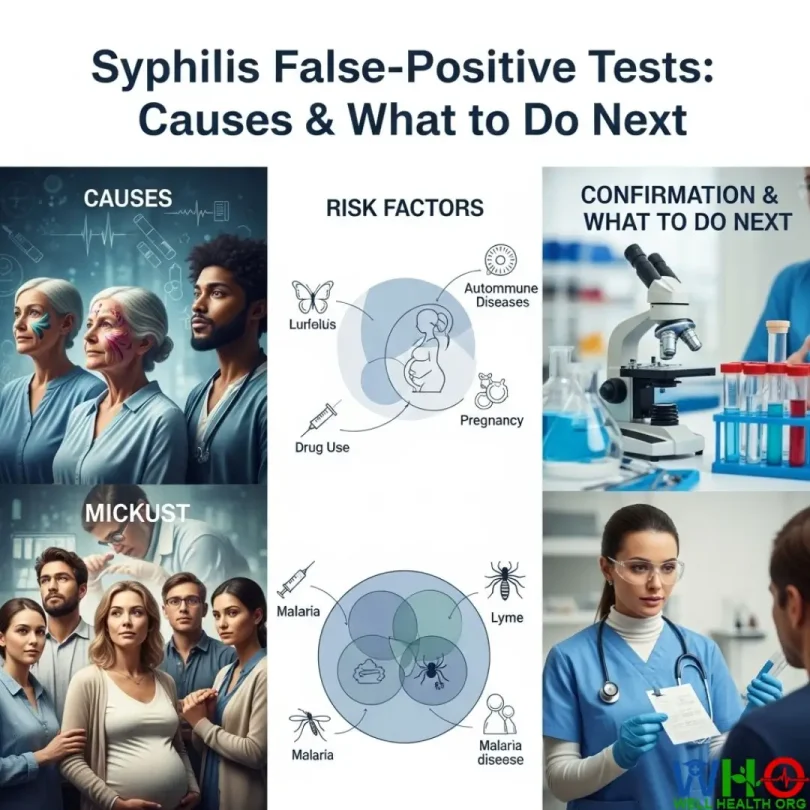
Receiving a positive test result for syphilis can feel shocking, overwhelming, and even frightening—especially if you have no symptoms or reason to believe you were exposed. What many people don’t realize is that false-positive results for syphilis are far from rare. These misleading outcomes can happen to anyone, regardless of age, gender, or lifestyle.
- Introduction Syphilis False-Positive Tests
- What Is a False-Positive Syphilis Test?
- Common Causes of False-Positive Syphilis Tests
- Autoimmune Diseases
- Pregnancy
- Other Infections
- Vaccinations and Medications
- Age-Related Factors
- Understanding Syphilis Test Types and Their Accuracy
- Nontreponemal Tests (Initial Screening)
- Treponemal Tests (Confirmatory Testing)
- Reverse Algorithm Testing
- Confirming an Accurate Syphilis Diagnosis
- Repeat Testing with Different Methods
- Clinical Evaluation
- Specialized Confirmatory Tests
- Emotional and Practical Implications of False-Positive Results
- Emotional Distress
- Unnecessary Treatment Concerns
- Relationship Impact
- Documentation and Privacy Issues
- Who Has Higher Risk for False-Positive Results?
- People with Autoimmune Conditions
- Pregnant Women
- People with Chronic or Recent Infections
- Older Adults
- Travelers or Residents in Endemic Regions
- Preventing and Managing False-Positive Results
- Provide a Complete Medical History
- Follow Recommended Testing Algorithms
- Seek a Second Opinion
- Stay Calm and Patient
- Moving Forward with Confidence
- Frequently Asked Questions About False-Positive Syphilis Tests
- How Common Are False-Positive Syphilis Results?
- Can Stress or Lifestyle Factors Cause False Positives?
- How Long Does It Take to Confirm Results?
- What Should I Do If My Partner Tests Positive but I Don’t Have Symptoms?
- Will a False Positive Stay on My Record Forever?
- Expert Tips for Coping With False-Positive Results
- 1. Ask Questions Immediately
- 2. Avoid Internet Panic
- 3. Manage Stress While Waiting
- 4. Keep Your Partner Informed
- 5. Seek Emotional Support
- Why Accurate Syphilis Testing Matters
- Protecting Public Health
- Preventing Overtreatment
- Improving Patient Trust
- Final Thoughts: Taking Control of Your Health
- FAQs
False positives can cause unnecessary emotional stress, relationship tension, and even lead to unneeded medical treatments. But with the right knowledge, you can better understand why they occur and how doctors confirm whether syphilis is truly present.
This detailed guide breaks down why false-positive results happen, what conditions and situations cause them, and how healthcare providers ensure accurate diagnoses. By the end, you’ll feel more equipped to approach syphilis testing with clarity instead of fear.
What Is a False-Positive Syphilis Test?
A false-positive syphilis test means your results suggest you have the infection when, in reality, you don’t. In other words, the test detects certain antibodies or markers in your blood that look like those produced in response to Treponema pallidum (the bacteria that causes syphilis), but those markers are actually triggered by something else.
Doctors generally divide test outcomes into two categories:
- Reactive (positive): The test detects antibodies, suggesting possible infection.
- Non-reactive (negative): No antibodies are detected, indicating no infection.
The confusion usually arises when the first test shows a reactive result, but follow-up tests reveal no evidence of syphilis. In these cases, the initial positive is considered false.
Medical studies have shown that false positives aren’t just rare mistakes—they happen more frequently than people expect:
- A 2019 study found that about 11% of reactive nontreponemal tests were actually false positives.
- According to the CDC, between 14% and 40% of treponemal tests done using the reverse testing method also yield false positives.
These statistics highlight the importance of not panicking after one positive test. Instead, additional testing is essential for an accurate diagnosis.
Common Causes of False-Positive Syphilis Tests
You may wonder—why would your body produce antibodies that make it look like you have syphilis when you don’t? Several medical conditions, life stages, and external factors can interfere with test results.
Here are the most common reasons:
Autoimmune Diseases
Autoimmune conditions are among the leading causes of false-positive syphilis results. In these disorders, the immune system mistakenly attacks healthy tissues, producing antibodies that may “confuse” diagnostic tests.
- Systemic Lupus Erythematosus (SLE): Up to 20% of lupus patients may test falsely positive for syphilis, even without ever having the infection. In one real-world case, a 34-year-old woman with lupus repeatedly tested positive on early screening but was later confirmed negative through specialized tests.
- Rheumatoid Arthritis (RA): This chronic inflammatory disease often leads to high levels of antibodies that cross-react with syphilis tests.
- Antiphospholipid Syndrome (APS): Known for increasing blood clot risks, APS also causes antibody production that interferes with screening accuracy.
Essentially, autoimmune diseases create a biochemical “background noise” that can trick certain blood tests into signaling infection when there is none.
Pregnancy
Pregnancy is another situation where false-positive results are relatively common. Due to hormonal changes and immune system adaptations, pregnant women may produce unusual antibody levels.
- Research indicates that 10–15% of pregnant women may experience a false-positive syphilis result during routine prenatal screening.
- Since syphilis testing is mandatory during pregnancy to protect both mother and baby, doctors face the challenge of acting quickly while also avoiding unnecessary treatments.
This is why confirmatory testing becomes particularly important for expectant mothers. A single reactive result doesn’t always mean infection—it may simply be a biological side effect of pregnancy.
Other Infections
Infections—both viral and bacterial—can also cause cross-reactivity in syphilis blood tests.
- Viral Infections: Conditions such as HIV, hepatitis C, and mononucleosis may trigger antibodies that interfere with syphilis testing.
- Parasitic Infections: Malaria, especially in regions where it is common, is notorious for causing false positives.
- Related Treponemal Infections: Diseases like yaws, bejel (endemic syphilis), and pinta, caused by bacteria closely related to Treponema pallidum, often trigger positive results even though they aren’t sexually transmitted.
This overlap occurs because the immune system produces very similar antibodies in response to these infections.
Vaccinations and Medications
Another surprising cause of false positives comes from certain vaccinations and medications.
- After vaccines, the immune system ramps up antibody production, which may sometimes cross-react with test markers. Though rare, some doctors have observed temporary false positives following vaccines, including newer ones like COVID-19 shots.
- Certain antipsychotic drugs and the use of intravenous (IV) drugs have also been linked to unusual antibody activity, though researchers are still investigating the exact mechanisms.
While uncommon, these scenarios remind us that not every positive result automatically means infection.
Age-Related Factors
As people age, their immune systems accumulate a history of past infections and antibody responses. Over time, this buildup can make it harder for tests to distinguish between genuine infection markers and harmless leftover antibodies.
- Older adults, therefore, have slightly higher chances of false-positive syphilis test results.
- Age-related changes in immune function further increase the possibility of cross-reactivity.
This is one reason why healthcare providers always consider a patient’s age and medical history when interpreting test results.
Understanding Syphilis Test Types and Their Accuracy
To fully grasp why false positives happen, it helps to understand the two main categories of syphilis tests and how they work. Each has its own strengths and limitations.
Nontreponemal Tests (Initial Screening)
These are usually the first-line tests used for screening:
- Rapid Plasma Reagin (RPR)
- Venereal Disease Research Laboratory (VDRL) test
Both detect antibodies produced in response to cellular damage caused by syphilis bacteria, rather than antibodies to the bacteria itself.
- Advantages: Quick, inexpensive, and effective for initial screening.
- Limitations: They are prone to false positives because many other conditions can cause similar antibodies to appear.
That’s why doctors rarely rely solely on these tests for a final diagnosis.
Treponemal Tests (Confirmatory Testing)
Treponemal tests look for antibodies specifically directed against Treponema pallidum. Common examples include:
- Fluorescent Treponemal Antibody Absorption (FTA-ABS)
- T. pallidum Particle Agglutination Assay (TP-PA)
- Chemiluminescence Immunoassays (CLIA)
- T. pallidum Enzyme Immunoassay (TP-EIA)
- Advantages: Far more accurate and specific than nontreponemal tests.
- Limitations: More expensive, take longer to process, and once positive, they usually stay positive for life—even after successful treatment.
This means treponemal tests confirm whether syphilis antibodies are present but can’t always distinguish between a current infection and a past, treated one.
Reverse Algorithm Testing
Traditionally, doctors used nontreponemal tests first, then confirmed positives with treponemal tests. However, many labs now use the reverse sequence:
- Start with a treponemal test.
- If positive, follow up with a nontreponemal test to check for active infection.
- Pros: This method can catch old, treated infections that might otherwise go unnoticed.
- Cons: It also increases the chances of false positives, making result interpretation more complex.
Ultimately, the testing approach depends on the lab, the patient’s medical history, and the healthcare provider’s judgment.
Confirming an Accurate Syphilis Diagnosis
A single positive test is never enough to confirm syphilis. Doctors use a combination of strategies to separate true infections from false positives.
Repeat Testing with Different Methods
If an initial test is positive, your doctor will likely:
- Order a confirmatory treponemal test if the first test was nontreponemal.
- Repeat testing at a different lab or with a different method.
- Request quantitative testing, which measures antibody levels to distinguish between ongoing infection and a false alarm.
This “double-check” process ensures results aren’t just lab errors or cross-reactions.
Clinical Evaluation
Lab results don’t tell the full story. Doctors always combine test outcomes with a patient’s medical background and physical signs:
- Do you have any visible symptoms, such as sores or rashes?
- Have you had any recent sexual exposures or risk factors?
- Do you have autoimmune conditions or recent infections that might explain the result?
This clinical context helps determine whether a positive test is truly meaningful.
Specialized Confirmatory Tests
In complicated cases—such as in patients with multiple autoimmune diseases—specialized confirmatory tests or expert consultations may be required. Infectious disease specialists and laboratory medicine experts often step in to help interpret tricky results.
By layering different testing strategies with careful evaluation, doctors can confidently confirm or rule out syphilis.
Emotional and Practical Implications of False-Positive Results
Testing positive for a sexually transmitted infection (STI) like syphilis can stir up a storm of emotions—even if the result turns out to be false. Beyond the medical aspect, these test results often carry personal, social, and psychological weight that people don’t expect.
Emotional Distress
One of the first and strongest reactions to a positive syphilis result is often fear and anxiety. For many people, an STI diagnosis feels deeply stigmatized. Questions such as “What will my partner think?” or “Will this affect my health permanently?” immediately come to mind.
Even when doctors reassure patients that the result could be false, the waiting period for confirmatory tests can feel like an eternity. This anxiety may also trigger physical symptoms like insomnia, nausea, or headaches, adding another layer of discomfort.
The stress is even greater for individuals in committed relationships. A positive syphilis test may cause someone to doubt their partner’s fidelity or worry about accusations of infidelity. Until a false positive is confirmed, relationships can become strained by suspicion and mistrust.
Unnecessary Treatment Concerns
Penicillin, the standard treatment for syphilis, is usually safe and effective. But unnecessary treatment—especially if it involves repeated injections or oral antibiotics—can have downsides:
- Allergic Reactions: Some people have penicillin allergies, which can cause anything from mild rashes to severe, life-threatening reactions.
- side effects: Even when tolerated, antibiotics can cause side effects like diarrhea, yeast infections, or stomach upset.
- Medical Burden: Receiving treatment for an infection you don’t have can be emotionally discouraging and undermine trust in healthcare providers.
For these reasons, confirmatory testing before starting treatment is critical. Doctors must weigh the risks of delaying treatment (in case syphilis is real) against the risks of treating unnecessarily.
Relationship Impact
When someone tests positive for syphilis, partners often become directly involved—whether through testing, treatment, or tough conversations. Even if the result is later shown to be false, the initial shock can cause relationship damage.
- Some partners may immediately assume infidelity.
- Others may feel ashamed or mistrustful, even after learning it was a false alarm.
- Couples may struggle with lingering doubts long after the medical issue is resolved.
Clear communication and support from healthcare providers are essential to prevent unnecessary conflict and misunderstanding in these situations.
Documentation and Privacy Issues
Another overlooked consequence of false-positive results is the paper trail they create.
- Once a positive test is recorded in a medical chart, it may remain there—even if later disproven.
- Insurance providers or employers (in rare healthcare-related jobs) may access parts of these records, creating unnecessary stigma.
- In countries with centralized medical systems, such documentation may even affect future screenings or eligibility for certain programs.
For patients concerned about privacy, discussing medical record handling with healthcare providers is important. Some clinics also offer confidential testing options to reduce these risks.
Who Has Higher Risk for False-Positive Results?
Not everyone faces the same likelihood of receiving a false-positive syphilis result. Certain groups of people—due to their medical conditions, age, or life stage—are more vulnerable.
People with Autoimmune Conditions
As mentioned earlier, autoimmune conditions often lead to unusual antibody activity. People living with:
- Lupus (SLE)
- Rheumatoid arthritis
- Antiphospholipid syndrome (APS)
are especially prone to false positives. These individuals should always inform their doctors about their diagnosis before undergoing syphilis testing. Doing so helps providers interpret results more carefully.
Pregnant Women
Because prenatal care includes mandatory syphilis screening, pregnant women face repeated testing throughout their pregnancy. Combined with pregnancy-related immune changes, this makes false positives relatively common in this group.
The stakes are high: untreated syphilis can pass from mother to baby (congenital syphilis), which is why doctors must act swiftly. Yet at the same time, unnecessary treatment isn’t ideal for mother or child. This balancing act makes pregnancy one of the most sensitive situations for false-positive management.
People with Chronic or Recent Infections
Individuals who already live with chronic viral infections, such as:
- HIV
- Hepatitis B or C
- Epstein-Barr virus (which causes mononucleosis)
may produce antibody patterns that mimic syphilis infection. Likewise, people who’ve recently recovered from acute infections may temporarily show false-positive results due to immune system overactivity.
Older Adults
The immune system changes with age. Seniors, particularly those with a long history of illnesses or multiple vaccinations, may show background antibody activity that complicates testing. As a result, older adults are at slightly greater risk of confusing results.
Travelers or Residents in Endemic Regions
People who have lived in or traveled to areas where non-syphilis treponemal infections (like yaws or bejel) are common may also test positive. Though these infections aren’t sexually transmitted, the antibodies they produce often cross-react in syphilis tests.
Preventing and Managing False-Positive Results
While it’s impossible to completely eliminate the chance of false positives, both patients and healthcare providers can take steps to reduce confusion and improve accuracy.
Provide a Complete Medical History
Patients can play an active role in improving test accuracy simply by being open and thorough with their doctors. Before testing, it’s wise to share:
- Any known autoimmune conditions (like lupus or RA).
- Recent vaccinations (including flu, COVID-19, or travel-related vaccines).
- Current medications, especially long-term prescriptions.
- Past syphilis infections or treatments.
This background helps providers interpret results in context, lowering the risk of misdiagnosis.
Follow Recommended Testing Algorithms
The CDC and other health organizations recommend a structured two-step testing process instead of relying on a single test. By combining screening with confirmatory tests, doctors can:
- Catch early infections without overdiagnosing.
- Reduce the number of false positives.
- Ensure treatment is only given when necessary.
If your doctor skips confirmatory testing, it’s reasonable to ask why and request additional testing before starting treatment.
Seek a Second Opinion
If test results don’t match your symptoms, history, or risk level, consider consulting another healthcare provider. Infectious disease specialists, in particular, have extensive experience handling confusing test results.
Additionally, testing at a different laboratory may provide clarity, since lab techniques and equipment can vary.
Stay Calm and Patient
Perhaps the most important advice: try to remain calm. False positives are common enough that doctors deal with them regularly. Panicking only adds stress without changing the outcome. Trust the process of confirmatory testing and clinical evaluation.
Moving Forward with Confidence
False-positive syphilis test results can feel like a rollercoaster—frightening at first, but often resolved with careful follow-up. Understanding why these results happen, who is most at risk, and how doctors confirm accurate diagnoses gives you the tools to face the process with confidence.
- False positives are common and don’t necessarily mean infection.
- Confirmatory testing and clinical evaluation are essential.
- Many conditions—from pregnancy to autoimmune diseases—can cause misleading results.
- Open communication with your healthcare provider ensures the best outcome.
Ultimately, modern syphilis testing is highly reliable when done correctly. By using multiple tests and considering your medical history, providers can separate false alarms from true infections with confidence.
If you’ve received a positive result, take a deep breath, avoid assumptions, and work with your doctor to clarify the situation. Most importantly, remember that you are not alone—many people experience false-positive results, and there are clear steps to resolve them.
Frequently Asked Questions About False-Positive Syphilis Tests
False-positive results often leave people with more questions than answers. Below, we’ll explore some of the most common concerns patients have when faced with confusing test outcomes.
How Common Are False-Positive Syphilis Results?
False positives are more common than most people realize. Studies suggest that:
- Up to 11% of nontreponemal tests may produce false positives.
- 14–40% of treponemal tests (when using reverse sequence screening) may also give misleading results.
In simpler terms, false positives are not rare mistakes—they are an expected part of the testing process. That’s why confirmatory testing always matters.
Can Stress or Lifestyle Factors Cause False Positives?
While stress alone doesn’t directly cause false positives, it can weaken the immune system and make people more vulnerable to infections or immune irregularities. These changes sometimes lead to unusual antibody activity that complicates testing.
Lifestyle factors like drug use, poor diet, or lack of sleep don’t directly cause false positives either, but they can contribute to infections or immune conditions that do.
How Long Does It Take to Confirm Results?
The timeline depends on the testing method:
- Nontreponemal tests (like RPR or VDRL) usually return results within a few hours to a couple of days.
- Treponemal confirmatory tests often take several days to a week, depending on the lab.
During this waiting period, patients often feel stressed, but the delay is necessary to ensure accurate results.
What Should I Do If My Partner Tests Positive but I Don’t Have Symptoms?
If your partner tests positive, don’t panic. Follow these steps:
- Encourage confirmatory testing—a single positive test isn’t enough.
- Get tested yourself, even if you feel healthy.
- Avoid making assumptions about fidelity or past exposures until results are confirmed.
- Seek medical guidance together to avoid miscommunication and unnecessary conflict.
Remember, false positives can happen to anyone, so it’s important not to jump to conclusions.
Will a False Positive Stay on My Record Forever?
In many cases, yes—once recorded, a positive test may remain in your medical history. However:
- Your doctor can also add notes clarifying that later confirmatory testing proved it false.
- If you’re concerned about privacy, consider discussing record-handling policies with your provider or using confidential clinics for STI testing.
Expert Tips for Coping With False-Positive Results
Learning that your test result may be inaccurate is frustrating. Here are some practical strategies to handle the emotional and medical side of false positives.
1. Ask Questions Immediately
Don’t be afraid to ask your doctor:
- Which type of test was used?
- What are the chances of a false positive in my case?
- What confirmatory testing is planned?
- How long will it take to get final results?
Clear answers can reduce fear and help you understand the next steps.
2. Avoid Internet Panic
Many people immediately turn to online forums after receiving a positive result. While the internet can provide useful information, it can also amplify fear by presenting worst-case scenarios. Instead, focus on reliable medical sources and conversations with your healthcare provider.
3. Manage Stress While Waiting
Waiting for results is often the hardest part. Techniques like deep breathing, exercise, journaling, or meditation can help manage anxiety. Talking with a supportive friend or counselor may also prevent unnecessary panic.
4. Keep Your Partner Informed
If you’re in a relationship, hiding the situation usually creates more stress. Instead, share what you know, explain that false positives are possible, and reassure your partner that confirmatory testing is underway. Honest communication builds trust during uncertain times.
5. Seek Emotional Support
A false-positive test isn’t just a medical issue—it can feel like a personal crisis. Support groups, therapists, or even online communities focused on sexual health awareness can provide comfort and reduce feelings of isolation.
Why Accurate Syphilis Testing Matters
Syphilis remains a serious infection worldwide. Left untreated, it can cause severe long-term complications, including neurological problems, heart damage, and in pregnant women, life-threatening risks for the baby. That’s why testing is essential—even if false positives sometimes occur.
Protecting Public Health
Accurate testing ensures that:
- Infections are caught early, before they spread to others.
- Pregnant women can be treated in time to prevent congenital syphilis.
- Public health agencies can monitor infection rates effectively.
Preventing Overtreatment
At the same time, accurate testing prevents unnecessary treatments. Antibiotics should be reserved for real infections to avoid side effects and reduce the risk of antibiotic resistance.
Improving Patient Trust
When doctors carefully confirm results before diagnosing, patients gain confidence in their healthcare providers. Trust is vital for ongoing STI prevention, treatment, and communication.
Final Thoughts: Taking Control of Your Health
Receiving a positive syphilis test result—especially if unexpected—can be one of the most stressful health experiences. But it’s important to remember that:
- False positives are common, especially among people with autoimmune diseases, pregnant women, and those with certain infections.
- Confirmatory testing is standard practice to ensure accuracy.
- Emotional distress is normal, but it can be managed with clear communication, patience, and support.
The key takeaway: a single positive test is not the end of the story. With modern testing protocols, skilled healthcare providers can almost always distinguish between a false positive and a true infection.
Your role as a patient is to stay informed, ask questions, and provide your full medical history. Doing so empowers you to make the best decisions for your health and reduces unnecessary worry.
So if you ever face a positive syphilis test result, remember—you are not alone, and it doesn’t necessarily mean you have the infection. Take a deep breath, trust the process, and know that clarity is just a follow-up test away.
FAQs
1. Can a false-positive syphilis test turn into a true positive later?
No. A false positive means you never had syphilis to begin with. However, if you are later exposed to the infection, you can still contract it. That’s why ongoing prevention and safe practices remain important.
2. How do doctors know if it’s really a false positive?
They use a combination of repeat tests, confirmatory treponemal testing, and clinical evaluation. If follow-up tests show no evidence of syphilis and you have no symptoms, the initial result is deemed false.
3. Should I tell my partner if I have a false positive?
Yes, honesty is usually the best approach. Explain that false positives are common and that you’re undergoing confirmatory testing. Sharing accurate information prevents unnecessary conflict.
4. Do false positives happen with other STIs?
Yes. HIV, hepatitis C, and herpes tests can also occasionally produce false positives, though testing protocols are designed to minimize this risk.
5. What’s the best way to prevent false positives?
You can’t always prevent them, but providing a full medical history, following recommended two-step testing, and seeking second opinions when needed greatly reduce the risk of misdiagnosis.
Medically Reviewed by Prof. Dr. Akram
Orthopedic Surgeon | Professor | Senior Medical Specialist
Prof. Dr. Akram is a distinguished surgeon with over 15 years of clinical expertise. Having served as a lead Emergency Specialist at Complex International Government Hospital, he currently leads a specialized team of 13 medical professionals at his private hospital. As a Professor at top medical universities, he ensures that every article on WellHealthOrg.com meets rigorous clinical standards.
Medical Disclaimer:
The information provided is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your physician for any medical concerns.
Our content is rigorously fact-checked by our 13-member Editorial Team under the clinical supervision of Prof. Dr. Akram.